Whooping cough – scientifically known as pertussis – is a highly contagious respiratory disease that especially threatens the health of infants. Whooping cough is spread via germ-filled droplets that are dispersed into the air through coughing and sneezing. This condition is often left undetected for around 5-10 days until the extensive coughing fits become apparent. If no precautions (such as timely vaccinations) are taken to obstruct the spread during this undetected stage, the condition is not only dangerous to the patient but also highly infectious.
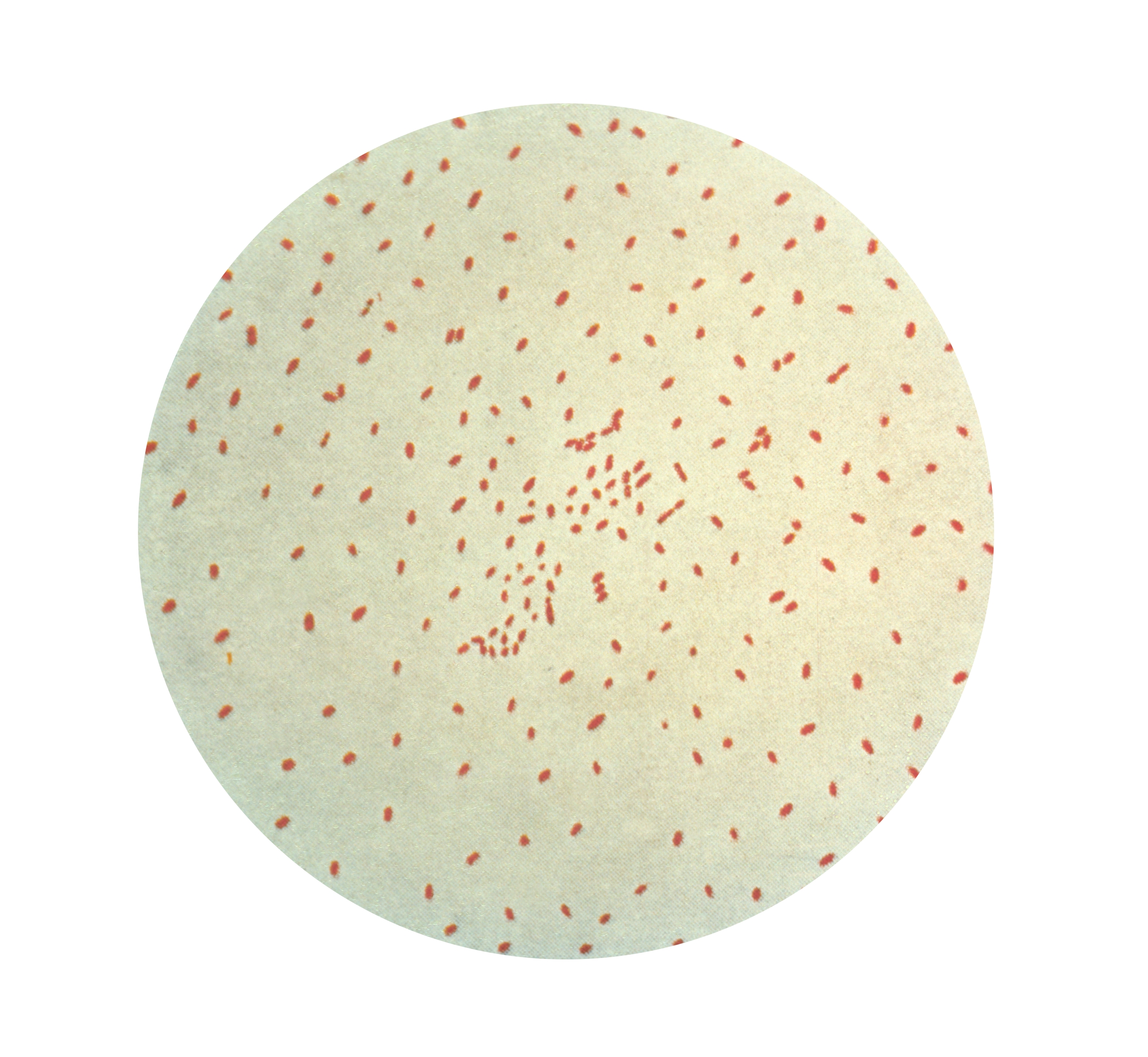
This disease is caused by Bordetella pertussis, a bacteria which attack the cilia, the fine hairs in the respiratory tract that allow self-cleansing of mucus in the airway. Toxins are then released causing airways to swell which disrupts the vital functions around the body, with time this can lead to serious health problems such as pneumonia, chronic vomiting, brain damage and fatal damage. The disease gets the name ‘whooping cough’ from the ‘WHOOP’ sound made when breathing in between coughs. The most significant symptom is a lasting and persistent cough which is emphasised by the nickname '100-day cough'.
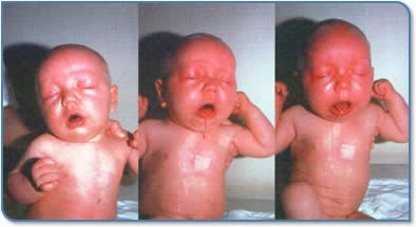
Whooping cough is particularly dangerous for little babies as the toxins can cause the blood vessels that go to their lungs to be constricted. With not enough blood going through the lungs, the babies will not get enough oxygen. Whooping cough is very hard to treat. “The patients face goes blue and sometimes they lose consciousness and there's simply nothing you can do.” (Grant, C. 16 May 2025).
With the disease so infectious and hard to treat, early prevention is vital. Prevention to ensure that the disease doesn’t spread and infect more young children, especially amongst the most vulnerable population (infants and babies) is critical. Young children under three months lack the ability to produce antibodies and protect themselves from the disease. "Around 50 percent of pēpi (babies) who catch whooping cough before the age of 12 months need hospitalisation and 1 or 2 in 100 of those hospitalised pēpi die from the infection,". (Reid M. RNZ, Nov 2024).
Prevention in New Zealand
Vaccination to prevent and protect against the spread of whooping cough was introduced in New Zealand in 1945. The vaccination schedule for babies now begins at 6 weeks of age with two further doses at 3 and 5 months of age and booster doses in childhood. However the introduction of the vaccine has not in New Zealand changed the time interval between epidemics as these continue every 3-4 years. As further prevention, in 2012 the Ministry of Health began recommending that pregnant women between 16 and 26 weeks of pregnancy should get vaccination against whooping cough as early prevention for their newborns. The mother produces antibodies that cross the placenta, protecting the baby from infection during their first months of life. Vaccination during pregnancy is important in helping preventing whooping cough in very young babies, the vulnerable population that are too young to receive the vaccine.
Despite the developments made in the prevention of whooping cough Professor Cameron Grant , considers that “the biggest epidemic might be the current 2025 one, as there is extremely low vaccination coverage - the lowest in my entire career - which puts more people at risk than ever before.” (Grant, C. 16 May 2025). Although the effectiveness of vaccination is proven there are areas where immunisation coverage is low in New Zealand. The threat of a whooping cough epidemic is serious.
In New Zealand, Māori and Pacific people and those from lower socio-economic groups are disproportionally affected by the effects of whooping cough. Difficulties with timely and affordable access to healthcare along with cultural and socioeconomical factors contribute to low vaccination rates. Household crowding may also be a contributing factor to the rapid spread of whooping cough and increasing the risk of transmission.
For Professor Cameron Grant (Starship paediatrician) the most effective solution is simple. Timely vaccination is crucial in the prevention of whooping cough. Vaccination was introduced in 1945 and during pregnancy in 2012 as very young babies are particularly vulnerable. Prevention is critical as there are very few effective treatments for infants., “If you're an infant, 60% chance that you end up in the hospital. If you end up in a hospital, you got a one in 10 chance of ending up in intensive care. And if you're not in intensive care, you got a one in six chance of dying or being with your brain or lung damage.” (Grant C. 16 May 2025)
Whooping cough is not only preventable, it is also the responsibility of our society to prevent it. Timely vaccinations, particularly during pregnancy, remain our strongest defence. What starts off as a light cough and a runny nose could result in the death of loved ones and in most cases, it is entirely preventable.
In 2025, Our Health Journeys continued our partnership with Saint Kentigern College in Auckland to challenge a number of students to conduct research into an aspect of the medical history of Aotearoa New Zealand. The students, ranging from Years 8-13, produced their research in written, oral, or video format and the top projects were chosen for publication to Our Health Journeys.